Gastrointestinal Symptoms and Diets in EDS

There is a lot of discussion over specific diets and their ability to treat gastrointestinal (GI) symptoms. Some of the diets you may have heard of include gluten-free, dairy-free, low FODMAP, Anti-GERD, low histamine, full elimination diet, low salicylate, low oxalate, and many others. How do you know if these diets can help you? To better navigate this, it is important to take a thorough inventory of the foods you are consuming, the GI symptoms you experience, your current emotional and physical state, and the time of onset for at least 1 week. Doing so can identify your specific trends and triggers for certain symptoms.
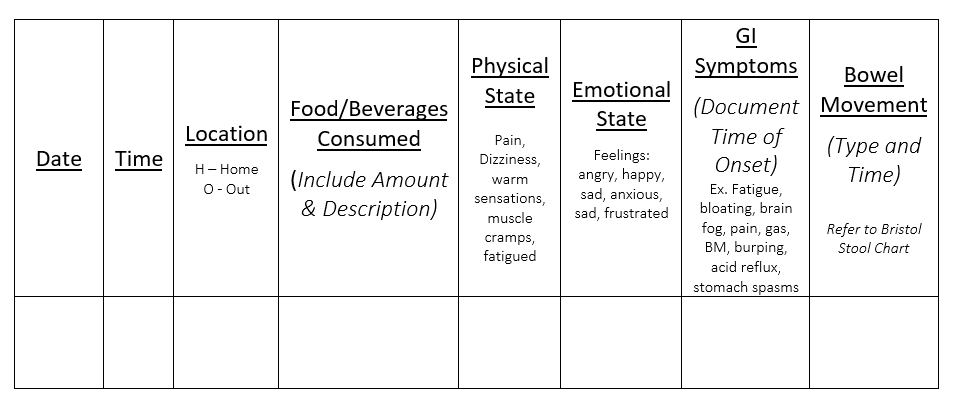
Below is an example of a food log that can be implemented:
When reviewing your weekly record there are some questions you may want to consider asking yourself before determining if a particular diet is appropriate for you. These can include:
- What is the overall quality of my diet?
- Am I incorporating foods that are anti-inflammatory?
- Am I incorporating foods that can have the potential to drive inflammation?
- Ex. Fried foods, hydrogenated oils, excessive intake of omega 6 oils (corn oil, sunflower oil, palm oil, etc), food dyes, sugar substitutes, excessive sugar intake, refined grains, etc.
- What is the timing between my meal intake?
- What are the portions of foods that I am able to tolerate?
- What was my physical and emotional state around mealtimes?
- Were GI symptoms present when physical and emotional symptoms were present either around mealtimes or during non-mealtimes?
If there are improvements you can make to the quality of your diet, meal timing and consistency, that may be a first place to start without implementing a specialized diet. If GI symptoms are present along with physical and emotional symptoms, more exploration into the causes and potential treatments of these symptoms can be considered prior to implementing specialized diets. Some examples can include:
- Potential electrolyte, blood sugar, and fluid imbalances with physical symptoms of nausea, dizziness or lightheadedness
- Quality of diet for pain control or other therapeutic measures to manage pain
- Potential mind-body practices for stress management to help stimulate the parasympathetic nervous system to help relax the gastrointestinal tract
If you review your food record and you notice a significant trend of GI symptoms with the intake of certain foods, investigate what component within that food or specific foods could you be most sensitive to. Trialing an elimination plan may provide some benefit. When taking this approach, we target a broad range and narrow it down as sensitivities of various foods can present with similar symptoms. Common suspects can include food proteins such as red meat, seafood, nuts, soy, eggs, gluten, dairy, and corn. We then go into different fermentable carbohydrates such as the Low FODMAP diet. If no improvement can be seen through these diets, then we start to look at chemicals that can be found within foods where a sensitivity may occur. These can include histamine, salicylate, oxalate, and many others. The type of diet chosen will depend on the foods consumed and the GI symptoms experienced. It is important to mention that a reaction to foods may not occur immediately following meals and can be delayed up to 72 hours. GI motility can also impact when a reaction may be experienced.
In some cases, GI symptoms may linger despite the type of diet chosen. While there is no confirmative mechanism that is known for why GI symptoms occur with EDS, an article published in the American Journal of Medical Genetics Part C (Seminars in Medical Genetics) entitled, “Gastrointestinal and Nutritional Issues in Joint Hypermobility Syndrome/Ehlers-Danlos Syndrome, Hypermobility/type” provides some theories. These can include laxity in the peritoneal ligaments of the gut apparatus, abnormal connective tissue in the gut wall of the muscularis externa and an extracellular matrix defect of the lamina propria. Our main goal with nutrition is to try and meet nutritional needs to optimize nutritional status while establishing a diet that can provide the most comfort without over restricting.
If you are having any difficulty on navigating diet and optimizing your nutritional intake while living with EDS, please don’t hesitate to reach out to your physician for a referral to see a dietitian knowledgeable in EDS. Please keep an eye out for an update to this post with new insights on the interaction between the gut-brain, proprioception, neuroception, and interoception with symptoms that may be experienced while living with EDS that can impact diet and nutritional status.
